Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Melioidosis in Si Sa Ket Model: Risk Factors with Prevention and Control
*Corresponding author: Choosak Nithikathkul, Tropical Health Innovation Research Unit, Faculty of Medicine, Mahasarakham University, Thailand.
Received: November 28, 2022; Published: December 07, 2022
DOI: 10.34297/AJBSR.2022.17.002374
Abstract
Melioidosis is a communicable disease caused by the gram-negative bacterium Burkholderia pseudomallei, usually found in soil, water, and mammals. This disease is highly prevalent in Southeast Asia and Northern Australia. The transmission spreads through percutaneous inoculation, inhalation, or ingestion, which is challenging to diagnose and treat. Therefore, the researcher’s findings on the prevalence of Melioidosis incidence in 2019 in one province area in Northeast Thailand showed that the distribution of disease-infected males was 67.9% with ages between 45-54 years ordinally infecting Thais 98.8%, and those engaged in agriculture 52.6 %, and with low health literacy at 32.6%. According to an analysis of factors affecting prevalence, the sample was 265 patients diagnosed by IHA/IFA in 2018-2019..
The study group was patients in high-prevalence areas, while the control group was residual in low-prevalence areas. The results showed that the majority of the samples, 67.17% were male, 31.32% were in agriculture, and 41.89% had underlying diseases. Univariate analysis found that the factors associated with the prevalence of disease in the area were: injury (p-value 0.003), house characteristics (p-valu =0.049), household environment (p-value 0.008), exposure to patients (p-value 0.012), smoking (p-value 0.001), alcohol consumption (p-value 0.001), underlying disease (p-value<0.014), rainy season (p-value 0.001), living in the area more than 20 years (p-value<0.017), perception of Melioidosis (p-value 0.001), perceived susceptibility (p-value<0.010) and perceived benefits (p-value<0.007). Multivariate analysis found that smoking, underlying disease, and season were associated with Melioidosis prevalence. Therefore, people living in high-risk areas should increase their knowledge about Melioidosis and disease prevention by wearing protective equipment, especially for smokers and people with chronic diseases. In addition, special disease control should be carried out during the rainy season. Finally, establishing people aware of the risk of the disease combined with disease surveillance should be carried out using a geographic map that monitors risk areas, especially at high prevalence with found Burkholderia pseudomallei in the environment can prevent and control Melioidosis appropriately for people at-risk area.
Keywords: Burkholderia pseudomallei, melioidosis, prevention and control
Introduction
Melioidosis is a contagious disease caused by the gramnegative bacterium of Burkholderia pseudomallei, commonly found in soil, water, and mammals. It is a highly prevalent disease in Southeast Asia and Northern Australia and is transmitted through percutaneous inoculation, inhalation, or ingestion [1-4]. Most infected patients are experiencing lung, joint, skin, hepatitis, and septicemia infections [5-9]. Sometimes, among patients infected with Burkholderia pseudomallei, more than 50% have a high chance of death. In addition, the bacteria can survive in acidic conditions at 24°C - 32°C, on water surfaces and at a depth of 60-90 cm deep under the soil surface [6,10].
The risk factors for Melioidosis include agricultural, and chronic diseases, especially diabetes, alcohol consumption, and smoking. In contrast, it was estimated that there would be an additional 165,000 cases per year and 89,000 deaths worldwide. No vaccine is also available to prevent them [5,10-15]./p>
According to the Department of Disease Control in Thailand, the morbidity rate has increased. In 2017, Thailand was the highest morbidity rate, with 13.32 per 100,000 population. (The morbidity rate was 5.21/100,000 population; the mortality rate was 0.18/100,000 population). Most infections were found in males, 67.9% between the age of 45-54 years old, and mainly in Thai (98.8%), doing agriculture activities, 52.6% as occupation, and low health literacy at 32.6%. Northeast Thailand is the province with a high incidence during the rainy season. Five areas initially had the highest morbidity rates: Mukdahan, Sisaket, Yasothon, Amnat Charoen and Ubon Ratchathani province.
For Burkholderia pseudomallei detection, the environment in high-prevalence areas was found in soil and water from fields or farms, wells, and swamps [16,17]. Thus, in regions with epidemics or high prevalence, disease prevention should be prevented by wearing protective equipment minimizing exposure to contaminated environments, and encouraging people to know about self-protection [12,18], especially those with wounds which should avoid direct contact with soil. The principles used in disease prevention and control established the measures when an epidemic occurs by government policies. However, a review of an outbreak in Sisaket province found that some areas had high incidence and prevalence while others could be protected and controlled. Therefore, the study would like to know the factors affecting the prevalence in the area and should develop preventive measures to control this outbreak.
Materials and Methods
Setting and study design. This study was a retrospective descriptive study. This is a study of outbreaks and factors affecting the prevalence of Melioidosis and a survey of pathogens detection in the environment from soil and water to the patient was exposed. The factors affecting the majority in the area. There were corrected data from hospitals; 265 Sisaket province patients were diagnosed by IHA/IFA method in 2019. They were divided into two groups: in the study group, 132 samples were from high prevalence areas, the control groups were 133 samples, and there were from low prevalence areas. The sample group used in the study had to be patients over 18 years, fully conscious and consenting to participate, not disabled, and able to read and write the Thai language. The exclusion criteria were those who had to undergo treatment or severe and unconscious symptoms.
Results
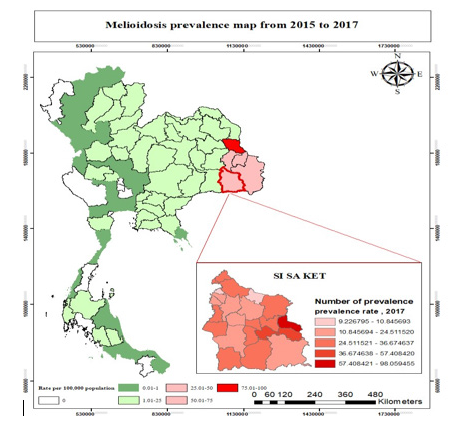
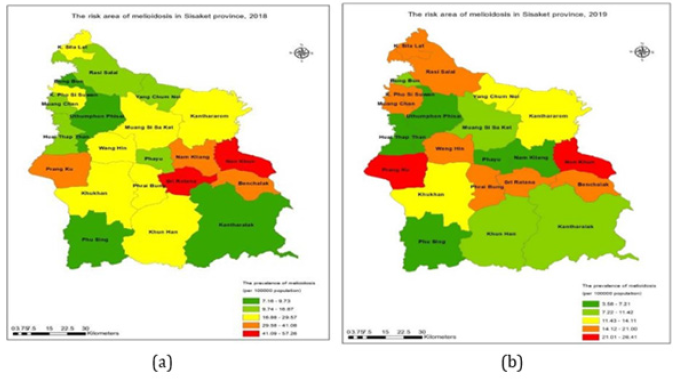
This study of the outbreak in Sisaket Province, Northeast Thailand, which aims to review the factors affecting the prevalence and developing guidelines for the prevention of Melioidosis, found that the areas have a high prevalence. Comparative analysis of the majority in 2015-2017 and incidence in 2018 - 2019 showed that the area with higher prevalence was Prangku and Srirattana and a constant majority in Nonkhun. This is shown in Figure 1-2.
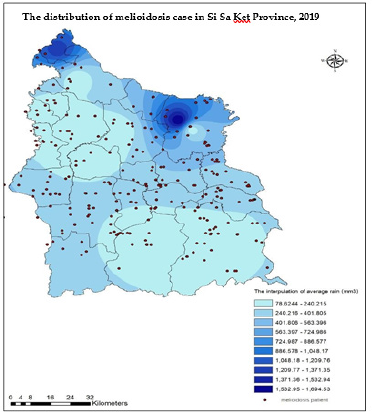
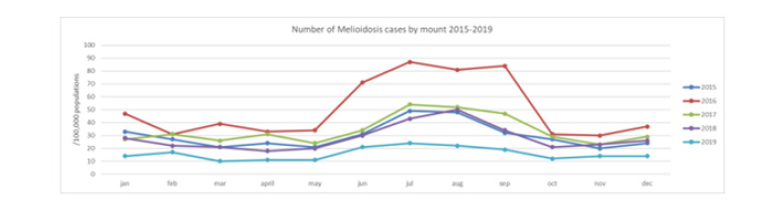
When studying the distribution of patients in areas with different rainfall, it was found that the patients were distributed in all areas. Nevertheless, it is more in areas with moderate rainfall. In areas with high rainfall, the distribution of patients was less. This is because the area is a reservoir with a large amount of water, so people in the area do not have direct contact with the soil and water sources, as shown in Figure 3. The study of the distribution of patients according to the season found that most cases increased between May - September and decreased from October-April. May - September is the rainy season. Patients have to go to farming areas and have a higher chance of being exposed to germs than in other seasons, increasing the number of patients, as shown in Figure 4.
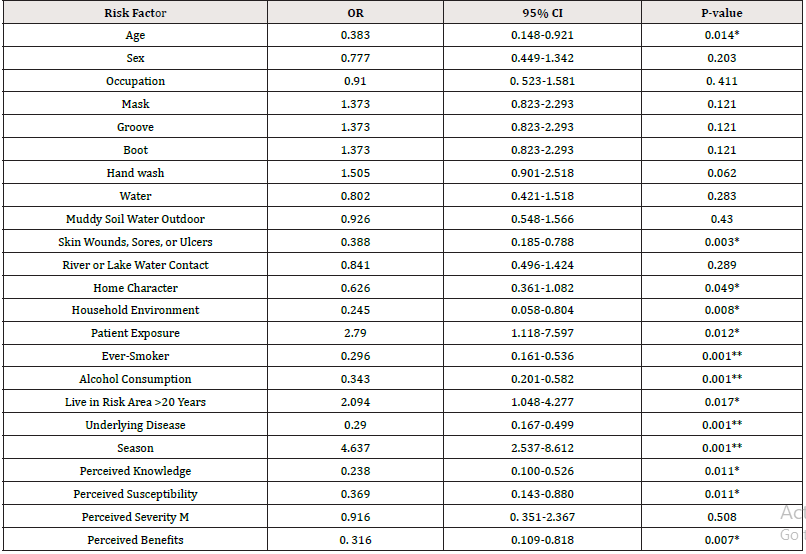
The 265 patients in Sisaket province with confirmed Melioidosis were majorly affected by males, 67.17% with agriculture-related activities, 31.32% and with underlying disease, 41.89%. The factors affecting the prevalence of Melioidosis in Sisaket Province include wound (p-value 0.003, 95%CI=0.185-0.788), Home character (p-value = 0.049, 95%CI= 0.36-1.082), household environment (p- value 0.008, 95%CI=0.058 - 0.804), patient exposure (p-value 0.012, 95%CI = 1.118-7.597), smoking (p-value 0.001, 95%CI =0.161-0.536), alcohol consumption (p-value 0.001, 95%CI = 0.201-0.582), underlying disease (p-value<0.014, 95%CI =0.167 - 0.499), season (p-value 0.001, 95%CI = 2.537-8.612), habitat in Sisaket more than 20 years (p-value<0.017, 95%CI = 1.04-4.277), perceived knowledge (p-value 0.001, 95%CI =0.100-0.526), perceived susceptibility (p-value<0.010, 95%CI =0.143-0.880) and perceived benefits (p-value<0.007, 95%CI = 0.109-0.818) as shown in Table 1.
Multi variable logistic regression of risk factors from table 1, p-value <0.05, such as age, skin wounds, sores, or ulcers, home character, household environment, patient exposure, ever-smoker, alcohol consumption, living in risk area >20 years, underlying disease, season, perceived knowledge, perceived susceptibility and perceived benefits. The input model found that factors of Melioidosis are people’s exposure to chronic illness, smoking, and the virus during the rainy season, as shown in Table 2.
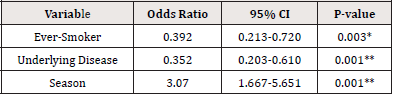
Table 2:Multivariable logistic regression of risk factors for expose Burkholderia pseudomallei (n=265).
1 Data shown as; p-value <0.05* and <0.001** 2 Multivariable logistic regression; Backward.
Discussion
In addition to factors affecting the prevalence of Melioidosis in Sisaket Province, the researcher studied the patient interviews and analysis of risk areas, and their coordinates were used in surveillance. This results in the factors affecting the prevention and control of Melioidosis. The plan especially changes personal behaviour in self-defense and reduces the severity and develops a model for prevention and control of Melioidosis in a risk area. The results of the study of 265 personal patients in Sisaket province with confirmed Melioidosis were found to affect males at 67.17%, with agriculture-related activities at 31.32% majorly and underlying disease at 41.89%. The factors revealed that factor age>40 years (P-value=0.014; OR=0.383,95%CI=0.148-0.921)[19] similar to Yazid et al.[19] study Melioidosis in ED were male gender, in working age group (40-59 year of age, 48.8 %) and a rainy season [19] and accordance with the education of others Factors associated with the incidence of Melioidosis was: working age, working in agriculture, and more cases were found in the rainy season [20-23]. Factor wounds (P-value=0.003; OR=0.388, 95%CI=0.185-0.788) Having an open wound can allow the infection to enter the body as easily as the study of Doker et al. [24].
A factor is an underlying disease (P-value=0.001; OR=0.290, 95%CI=0.167-0.499). It is mainly found in diabetes mellitus, chronic kidney disease and thalassemia. Chronic diseases lower the immune system, so the infection is more likely to enter than people without chronic diseases, such as diabetes, who cannot control blood sugar levels easily. The infection can enter the body more than normal people and cause other complications, following the higher intensity than the others [21,25-27]. Factor smoking (P-value=0.001; OR=0.296 95% CI=0.161-0.536) and alcohol consumption (P-value=0.001; OR =0.343, 95% CI=0.201-0.582) similar to limmathurotsalul, affected the prevalence of Melioidosis in the area. Because smoking and alcohol consumption makes it easier for B.pseudomallei to enter the body, such as smoking or drinking while working [28] but not similar to Hassan and Vandana, no significant associations between case-patients and either alcohol use or smoking [29,30]. This was consistent with several studies of risk factors for the disease, mainly due to individual characteristics [12,30,31], especially those with diabetics who were at higher risk of infection than normal people [26,30]. This study showed that wearing protective equipment such as Face masks, Boots and gloves has no conscious significance, similar to Vandana et al. [29]. However, washing your hands or cleaning immediately after work can also prevent this disease. There were other factors such as perceived knowledge (P-value=0.011; OR=0.238, 95%CI=0.100- 0.526), perceived susceptibility (P-value=0.011; OR=0.369, 95%CI=0.143-0.880) perceived benefits. (P-value=0.007; OR=0.316, 95%CI=0.109-0.818) perceptions of various aspects enable patients to understand and access disease prevention and control [32,33]. It shows that perceived knowledge, susceptibility, and perceived benefits affected personal behaviour change.
As for the environmental factors, such as soil and water near the household environment (P- value=0.008; OR=0.245, 95%CI=0.058- 0.804) and living in a risk area >20 years(P-value=0.017; OR=2.094, 95%CI=1.048 - 4.277), a house that is entirely protected against dust was more resistant to germs than a basement house, and an increase in travelers moving to and from endemic regions may result in an increased frequency of imported Melioidosis as well as being in an area with an outbreak for a long time The disease can transmit to human, it also has an incubation period from the first infection to 20 years [16,31,34-41]. This depends on climatic factors such as wind speed or storms that can carry pathogens contaminating airborne particulate matter to the house [1,23,35,37]. While the rainy season factor (P-value=0.001; OR=4.637, 95%CI=2.537 - 8.612) affected the prevalence of Melioidosis because farmers cultivate rice with water as a barrier to prevent the spread and the chance of infection [12,22,23,42]. When analyzed by backward multivariable logistic regression, it was found that smoking (OR=0.392, 95%CI=0.213- 0.720), underlying disease (OR=0.352, 95%CI=0.203 - 0.610) and the rainy season (OR=3.070,95%CI= 1.667-5.651) were the factors affecting the prevalence of diseases [28].
Therefore, prevention and control were developed to exercise surveillance on people with chronic and frequent smokers and active case finding, especially during the rainy season. The study of environmental factors showed that the pathogens in soil and water from areas of the interviewees were exposed in the five districts with the highest prevalence of Melioidosis confirmed the outbreak in the area. [18,29,41,43]. In addition, making a map showing the risk area will raise awareness among people in the area, and the coordinates of the infection to be monitored within a radius of 5-10 kilometres [17]. Currently, soil and water trading can transfer the germ to another site. While the coordinates from people’s behaviour modification will help reduce the morbidity in the area.
Conclusion
This study is a retrospective descriptive study to determine the factors affecting the prevalence of Melioidosis which is beneficial for planning the development of the model of Melioidosis prevention and control, especially in people who belong to at-risk groups such as people with chronic diseases and smokers that were living in high prevalence areas. The most suitable protection was to wear protective equipment at work. Moreover, during the rainy season, it is advised that more surveillance measures for Melioidosis at the same time the active case screening as an initial risk assessment. In addition, the map shows the risk area and encourages people to be aware of the risk of disease, while a rapid response network should be reported on and on-site urgently.
Funding
Please add: This research was funded by Mahasarakham University.
Institutional Review Board Statement
The study was approved by the research ethics Mahasarakham University (protocol code 149/2019 and date of approval 21 August 2019.
Informed Consent Statement
Patient consent was waived due to REASON “Written informed consent has been obtained from the patient(s) to publish this paper”
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to privacy.
Acknowledgements
We would like to thank the participants and staff from the public office of Sisaket province for their encouragement. Special thanks for a partial grant from Research Affairs Division, Faculty of Medicine and Tropical and Parasitic Diseases Research Unit, the Faculty of Medicine, Mahasarakham University. And Department of Microbiology and Immunology, Faculty of Tropical Medicine, Mahidol University for collaboration.
Informed Consent Statement
The authors declare no conflict of interest
References
- Bulterys PL, Michelle AB, Koukeo P, Manophab L, Mayfong M, et al. (2018) Climatic drivers of melioidosis in Laos and Cambodia: a 16-year case series analysis. The Lancet Planetary Health 2(8): 334-343.
- Control C f D (2015) Melioidosis. Northern Territory Government.
- Perumal Samy R, Bradley GS, Gautam Sethi, Lina H K Lim (2017) Melioidosis: Clinical impact and public health threat in the tropics. PLoS Negl Trop Dis 11(5): e0004738.
- Naha K, BA Shastry, K Saravu (2014) Colonization or spontaneous resolution: Expanding the role for Burkholderia pseudomallei. Asian Pacific Journal of Tropical Medicine 7(3): 250-252.
- Khiangte HL, Leena RV, Balaji V, Binesh Lal Y, Reka K, et al. (2019) Can the imaging manifestations of melioidosis prognosticate the clinical outcome? A 6-year retrospective study. Insights Imaging 10(1): 17.
- Teparrukkul P, Jiraphorn N, Susanna Dunachie, Direk L (2017) Clinical Epidemiology of Septic Arthritis Caused by Burkholderia pseudomallei and Other Bacterial Pathogens in Northeast Thailand. Am J Trop Med Hyg 97(6): 1695-1701.
- Stolt C, Imke HES, Yana Sayfart, Ivo Steinmetz, Antje Bast, et al. (2016) Heme Oxygenase-1 and Carbon Monoxide Promote Burkholderia pseudomallei Infection. J Immunol 197(3): 834-846.
- West TE, Nicolle DM, Direk L, HD Liggitt, Narisara C, et al. (2010) Pathogenicity of high-dose enteral inoculation of Burkholderia pseudomallei to mice. Am J Trop Med Hyg 83(5): 1066-1069.
- Panida Kanaphun, N Thirawattanasuk, Y Suputtamongkol, P Naigowit, D A Dance, et al. (1993) Serology and Carriage of Pseudomonas pseudomallei: A Prospective Study in 1000 Hospitalized Children in Northeast Thailand. The Journal of Infectious Diseases 167: 230-233.
- Cheng AC, BJ Currie (2005) Melioidosis: epidemiology, pathophysiology, and management. Clin Microbiol Rev 18(2): 383-416.
- BMJ Best Practice (2018) Melioidosis and glanders.
- BJ Currie, D A Fisher, D M Howard, J N Burrow, D Lo, et al. (2000) Endemic Melioidosis in Tropical Northern Australia: A 10-Year Prospective Study and Review of the Literature. Clinical Infectious Diseases 31(4): 981-986.
- Limmathurotsakul D, SJ Peacock (2011) Melioidosis: a clinical overview. Br Med Bull 99: 125-139.
- Peacock SJ, Direk L, Yoel Lubell, Gavin C K W Koh, Lisa J White, et al. (2012) Melioidosis vaccines: a systematic review and appraisal of the potential to exploit biodefense vaccines for public health purposes. PLoS Negl Trop Dis 6(1): e1488.
- Chantratita N, Vanaporn W, Direk L, Mongkol V, Aunchalee T, et al. (2008) Genetic diversity and microevolution of Burkholderia pseudomallei in the environment. PLoS Negl Trop Dis 2(2): e182.
- Seng R, Natnaree S, Rungnapa P, Christine JB, Sarika B, et al. (2019) Prevalence and genetic diversity of Burkholderia pseudomallei isolates in the environment near a patient's residence in Northeast Thailand. PLoS Negl Trop Dis 13(4): e0007348.
- Maude RR, Richard JM, Aniruddha G, Md Robed A, Md Belalul Islam, et al. (2012) Seroepidemiological surveillance of Burkholderia pseudomallei in Bangladesh. Trans R Soc Trop Med Hyg 106(9): 576-578.
- Allen C Cheng, Susan PJ, Linda Ward, Bart J Currie (2008) Melioidosis and Aboriginal seasons in northern Australia. Transactions of the Royal Society of Tropical Medicine and Hygiene 102(1): 26-29.
- Yazid MB, Mohd Hashairi F, Habsah H, Abu Yazid Md N, Zakuan Z D, et al. (2017) An 11-Year Analysis of Emergency Presentations of Melioidosis in Northeastern Malaysia. J Immigr Minor Health 19(3): 774-777.
- Philip L Bulterys, MA Bulterys, Koukeo P, Manophab L, Mayfong Mayxay, et al. (2018) Climatic drivers of melioidosis in Laos and Cambodia: a 16- year case series analysis. Lancet Planet Health 2(8): 334-343.
- Zainal Abidin H, Alwi Muhd B, Chandran N, Wan Fadzlina WS, Mohd Zulfakar M, et al. (2017) Acute bacteremic pneumonia due to melioidosis developing in the intensive care setting. IDCases 8: 63-65.
- Bart J Currie, Susan P Jacups (2003) Intensity of Rainfall and Severity of Melioidosis, Australia. Emerging Infectious Diseases 9(12): 1538-1542.
- WenChien Ko, Bruno Man HC, Hung Jen T, Hsin I Shih, Yeu Jun Lau, Li Rong W, et al. (2007) Melioidosis Outbreak after Typhoon, Southern Taiwan. Emerging Infectious Diseases 16(6): 896-898.
- Doker TJ, Tyler M Sharp, Brenda Rivera G, Janice PP, Tina J Benoit, et al. (2015) Contact investigation of melioidosis cases reveals regional endemicity in Puerto Rico. Clin Infect Di 60(2): 243-250.
- Stewart JD, Simon Smith, Enzo Binotto, William J Mc Bride, Bart J Currie, et al. (2017) The epidemiology and clinical features of melioidosis in Far North Queensland: Implications for patient management. PLoS Negl Trop Dis 11(3): e0005411.
- Antony G Faa, Peter J Holt (2002) Melioidosis in the Torres Strait Islands of Far North Queensland. Communicable Diseases Intelligence 26(2): 279-283.
- Dan M (2015) Melioidosis in Travelers: Review of the Literature. J Travel Med 22(6): 410-414.
- Limmathurotsakul D, Manas Kanoksil, Vanaporn Wuthiekanun, Rungrueng Kitphati, Bianca deStavola, et al. (2013) Activities of daily living associated with acquisition of melioidosis in northeast Thailand: a matched case-control study. PLoS Negl Trop Dis 7(2): e2072.
- Vandana KE, Chiranjay M, Chaitanya T, Asha Kamath, Meghan Tipre, et al. (2016) Seroprevalence of Burkholderia pseudomallei among Adults in Coastal Areas in Southwestern India. PLoS Negl Trop Dis 10(4): e0004610.
- Abu Hassan MR, Norasmidar Aziz, Noraini Ismail, Zainab Shafie, Benjamin Mayala, et al. (2019) Socio-epidemiological and land cover risk factors for melioidosis in Kedah, Northern Malaysia. PLoS Negl Trop Dis 13(3): e0007243.
- Jilani MS, Jamshedul Alam Md R, Md Mohiuddin, Md Rokib Hasan, Chowdhury Rafiqul A, et al. (2016) Burkholderia pseudomallei: Its Detection in Soil and Seroprevalence in Bangladesh. PLoS Negl Trop Dis 10(1): e0004301.
- Suntornsut P, Nittayasee W, Mayura M, Rungreung K, Susan M, et al. (2016) Barriers and Recommended Interventions to Prevent Melioidosis in Northeast Thailand: A Focus Group Study Using the Behaviour Change Wheel. PLoS Negl Trop Dis 10(7): e0004823.
- Chansrichavala P, Nittayasee W, Suthee S, Mayura M, Maliwan H, et al (2015) Public awareness of melioidosis in Thailand and potential use of video clips as educational tools. PLoS One 10(3): e0121311.
- Duangurai T, N Indrawattana, P Pumirat (2018) Burkholderia pseudomallei Adaptation for Survival in Stressful Conditions. Biomed Res Int 2018: 3039106.
- Timothy JI, S C Garrow, M Henderson, A Clair, J Sampson, et al. (2000) Burkholderia pseudomallei Traced to Water Treatment Plant in Australia. Burkholderia pseudomallei Traced to Water Treatment Plant in Australia 6(1): 56-59.
- Chandrakar S, M Dias (2016) Clinico-epidemiological spectrum of melioidosis: a 2-year prospective study in the western coastal region of India. Southern African Journal of Infectious Diseases 31(1): 14-19.
- Bart j Currie, M Mayo, N M Anstey, P Donohoe, A Haase, et al. (2001) A Cluster of Melioidosis Cases from An Endemic Region Is Lonal And Is Linked To The Water Supply Using Molecular Typing of Burkholderia Pseudomallei Isolates. Am J Trop Med Hyg 65(3): 177-179.
- Chuah CJ, Esther KHT, Rasana W, Alan D Ziegler (2017) Hydrological connectivity and Burkholderia pseudomallei prevalence in wetland environments: investigating rice-farming community's risk of exposure to melioidosis in North-East Thailand. Environ Monit Assess 189(6): 287.
- Kong Z, Y Fang, M Zhang, J Hong, Z Tan, et al. (2016) Melioidosis acquired by a traveler from Papua New Guinea. Travel Med Infect Dis 14(3): 267-270.
- Saidani N, Karolina Griffiths, Matthieu Million, Philippe Gautret, Gregory Dubourg, et al. (2015) Melioidosis as a travel-associated infection: Case report and review of the literature. Travel Med Infect Dis 13(5): 367-381.
- McRobb E, Derek S Sarovich, Erin P Price, Mirjam Kaestli, Mark Mayo, et al. (2015) Tracing melioidosis back to the source: using whole-genome sequencing to investigate an outbreak originating from a contaminated domestic water supply. J Clin Microbiol 53(4): 1144-1148.
- Currie BJ, Erin P Price, Mark Mayo, Mirjam K, Vanessa T, et al. (2015) Use of Whole-Genome Sequencing to Link Burkholderia pseudomallei from Air Sampling to Mediastinal Melioidosis, Australia. Emerg Infect Dis 21(11): 2052-2054.
- Lin Y, Qiang Wu, Xiang Liu, Sufang Dong, Lixian Wu, et al. (2016) Molecular tracking investigation of melioidosis cases reveals regional endemicity in Hainan, China. Biomed Rep 5(6): 766-770.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.